Reverse Shoulder Replacement
What to know about Reverse shoulder replacement surgery
A Patient’s Guide
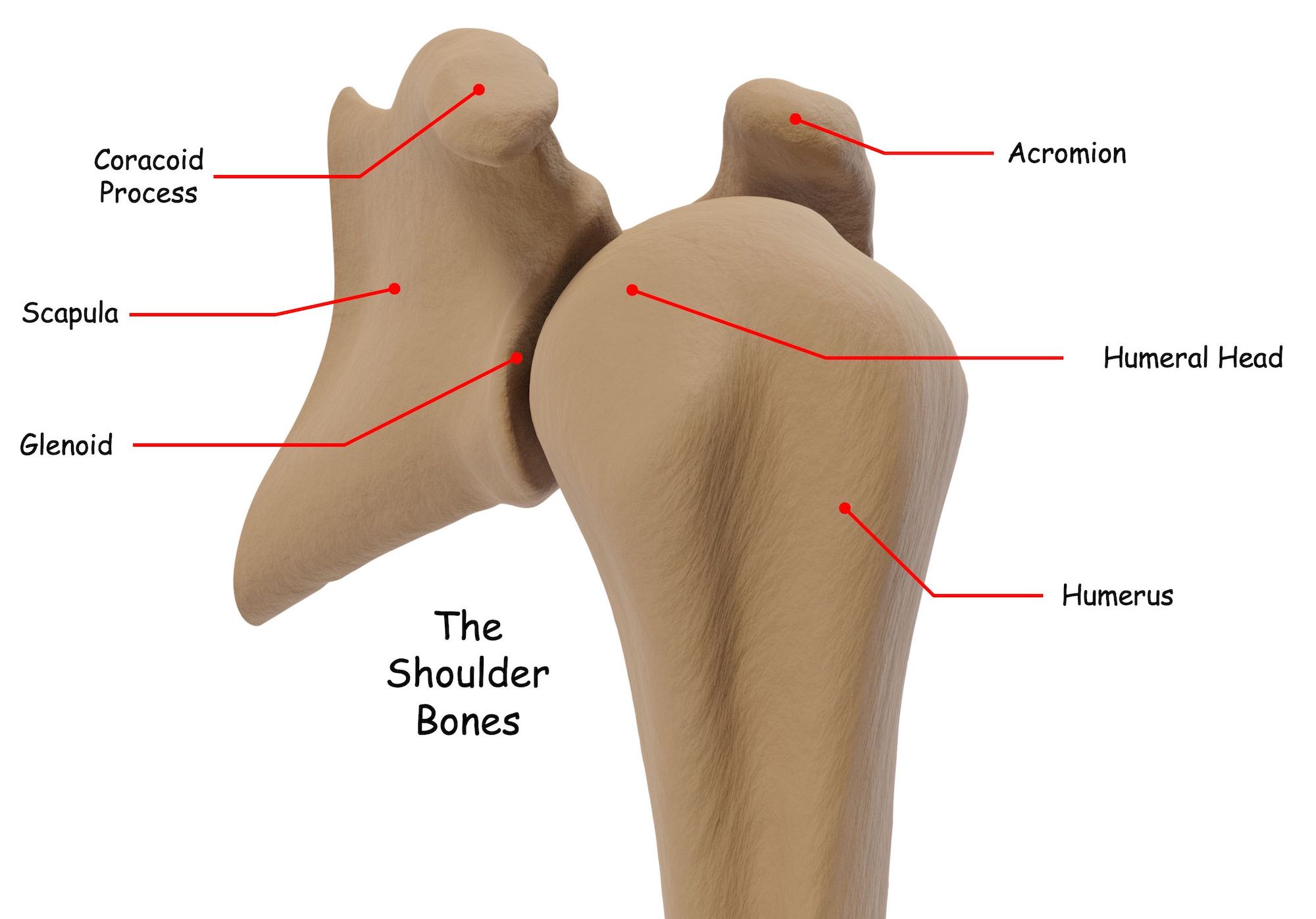
What makes up your shoulder anatomy?
What common shoulder joint conditions are treated with reverse shoulder replacement surgery?
- Large rotator cuff tears.
- Shoulder pain caused by shoulder arthritis.
- Large rotator cuff tears with arthritis, called cuff tear arthropathy.
- Complex shoulder fractures.
Large rotator cuff tears: When there is a large tear in the rotator cuff, the shoulder joint can become unstable and motion may be limited or completely restricted. If the tear is large enough, the humerus can dislocate, escape from the rotator cuff capsule and migrate up towards your clavicle or collar bone. If it migrates high enough it will contact part of the scapula called the acromion, a bone that does not have a layer of smooth articular cartilage. When the humeral head contacts the acromion it can cause significant shoulder pain and make shoulder movement difficult or impossible.
Arthritis: Over time the smooth lining or articular cartilage of the humeral head and glenoid wears. It can even wear out completely. As years go by, the articular cartilage thins and breaks down to a point where smooth, efficient, pain free movement is no longer possible. Generally, when the articular surface wears out, the shoulder joint becomes painful and movement is restricted. This condition is called arthritis and it is one of the most common reasons a surgeon would recommend a shoulder replacement. It is caused by wear and tear on the shoulder joint over many years of use.
“CTA” or Cuff Tear Arthropathy: If there is a large rotator cuff tear and arthritis at the same time, the condition is called cuff tear arthropathy or the acronym “CTA”. People with CTA often experience significant shoulder pain and extremely limited shoulder motion. In severe cases shoulder motion may be completely restricted. This is condition called pseudo-paralysis of the shoulder.
Shoulder Fractures: If someone has a severe shoulder fracture, they may be treated with a reverse shoulder replacement.
How are large rotator cuff tears and cuff tear arthropathy (CTA) managed?
- Initially, with conservative treatments like physical therapy.
- Shoulder pain may treated with medications.
- In severe cases, with reverse shoulder replacement.
Initially, cuff tears and CTA are managed with conservative treatments like physical therapy and restricted activities. If the shoulder pain is severe, nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids may be prescribed. Corticosteroids are powerful anti-inflammatory drugs that can be taken by mouth or injected into your shoulder.
However, when conservate treatment gives way to surgical intervention and shoulder replacement is recommended, the implant used is called a reverse shoulder replacement.
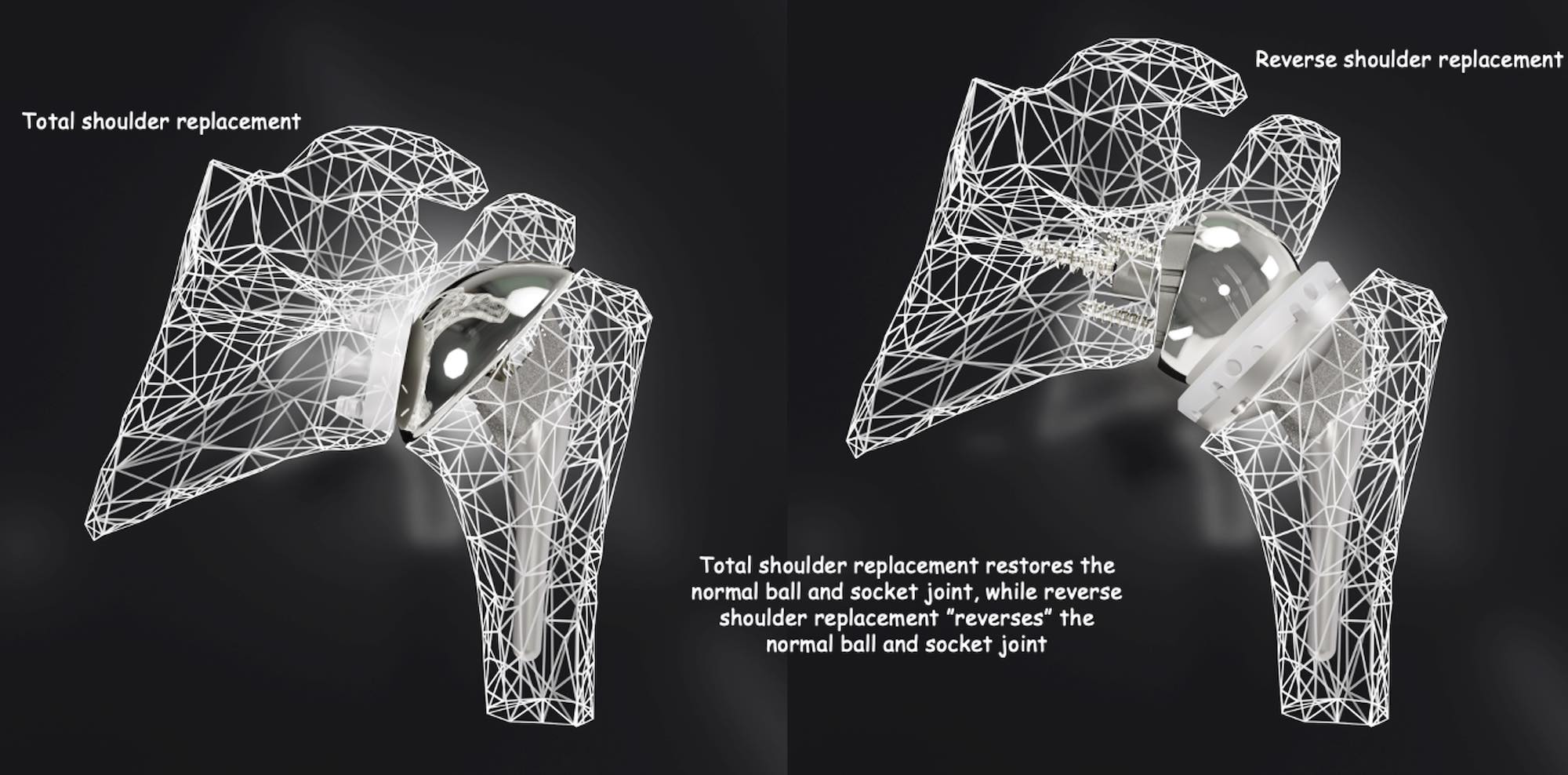
Like the normal shoulder anatomy, a reverse shoulder replacement is a ball and socket joint except the “ball” is placed on the glenoid side and the “socket” is placed on the humeral side. This configuration is the “reverse” or opposite of the normal shoulder anatomy, and that’s how it got its name! After reverse shoulder replacement or reverse shoulder arthroplasty, another word for “replacement”, and a full recovery, you should once again be able to raise your arm and perform normal daily activities with little or no shoulder pain.
How is shoulder arthritis managed?
- Initially, with conservative treatments like physical therapy.
- Shoulder pain may treated with medications.
- Severe cases in elderly patients may be treated with reverse shoulder replacement
Shoulder arthritis can cause significant shoulder pain, and it can become more severe over time, limiting what a person can do with their shoulder joint. Typically, non-surgical treatments are recommended first. Certain types of physical activities may be limited or restricted, and physical therapy may be recommended. Physical therapy is essential when treating arthritis and can be an effective way to reduce shoulder pain, improve shoulder motion and delay the need for shoulder surgery. As shoulder pain becomes more severe, nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids may be prescribed.
When conservative, non-surgical treatments no longer provide adequate shoulder pain relief and daily activities like getting a good night sleep, getting dressed, brushing your teeth, combing your hair, reaching behind your back, or playing golf, tennis or similar activities become difficult or impossible, or if you are elderly, a reverse total shoulder replacement may be recommended.
How you may benefit from reverse shoulder replacement surgery?
- Reduced shoulder pain.
- Improved strength and shoulder motion.
- A return to normal daily activities and a more active lifestyle.
There are significant benefits from a reverse shoulder replacement for CTA, large rotator cuff tears, or arthritis. These conditions not only cause significant shoulder pain, they make shoulder motion difficult or impossible and normal daily activities are extremely restricted or no longer possible.
A reverse shoulder implant is very unique and quite special! It not only relieves shoulder pain, it restores shoulder motion and this is what makes it different from other types of joint replacements like total shoulder replacement, knee replacement and hip replacement.
These types of implants are used primarily for pain relief and still depend on a person’s muscles, tendons and ligaments to facilitate movement. If someone has a large rotator cuff tear or CTA, restoring motion is something a traditional total shoulder replacement does not do well because typically, the rotator cuff muscles and tendons are no longer able to support and move the shoulder joint. A reverse shoulder replacement is the only joint replacement implant that can restore motion when the muscles and tendons that provide that motion are no longer functional. This is what makes reverse shoulder replacement revolutionary. People receiving a reverse shoulder arthroplasty typically experience dramatic improvements in their quality of life!
What advanced reverse shoulder replacement technology can benefit you today?
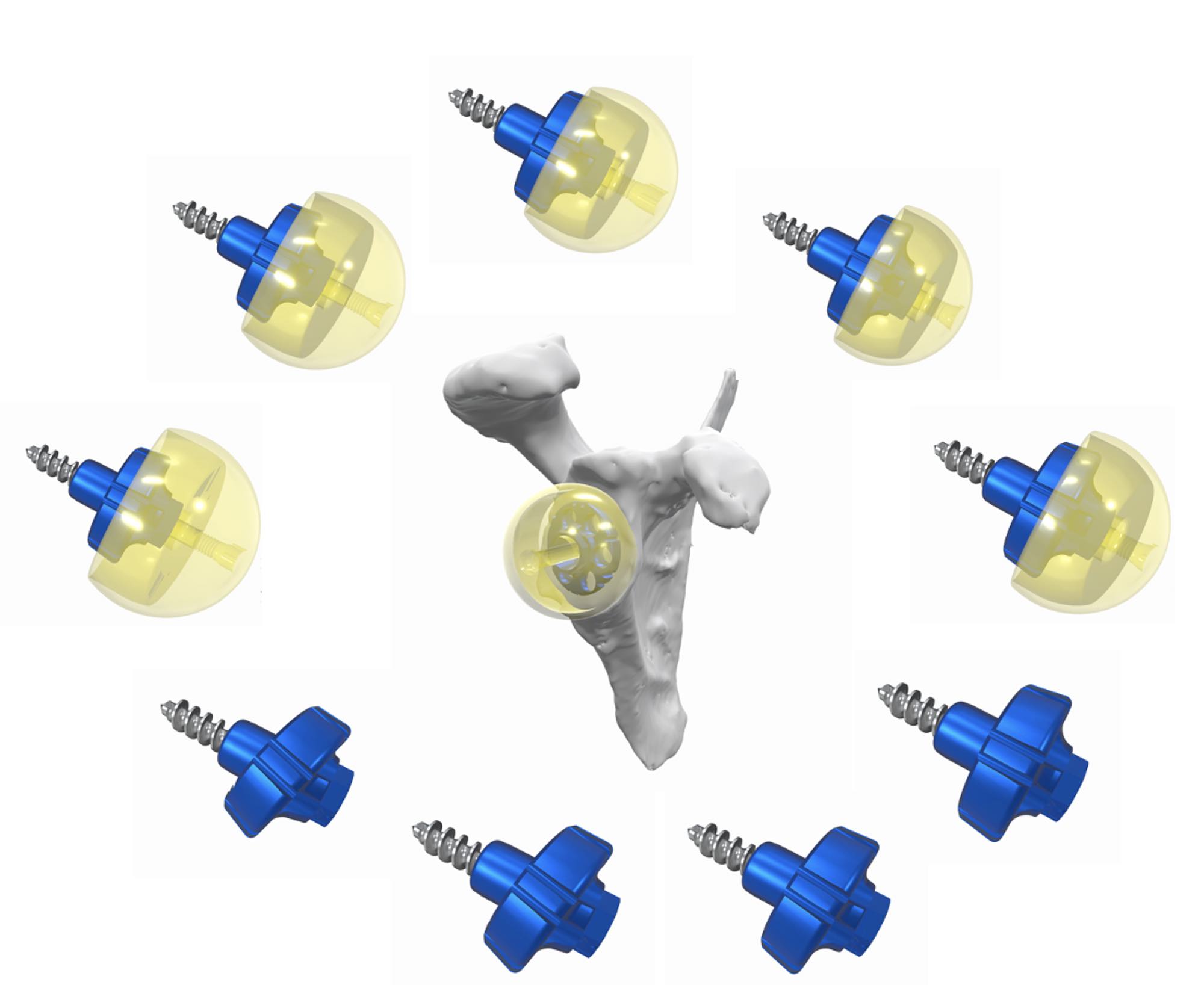
The InSet™ titanium (Ti) alloy Reverse Shoulder System is engineered to help patients achieve improved shoulder motion in the presence of a large rotator cuff tear with or without arthritis, maximize its potential longevity and preserve significant bone.
The InSet™ Reverse Shoulder System’s extensive implant options allow surgeons to choose the best combination of components based on a person’s unique anatomy and condition. With these options, surgeons can tailor fit their patients with components that give them the best chance for optimized shoulder motion and reduced complication risk.

How long a shoulder implant lasts is also dependent on how stabile the component remains over time. The InSet™ titanium (Ti) humeral stems feature three unique fins that are curved and coated with a titanium (Ti) porous material that promotes bone regeneration and bonding. These two features work together to improve stability and the potential for increased shoulder replacement longevity.

Another way to improve the longevity of shoulder replacement is through placement and alignment optimization, which may be done by allowing your surgeon to evaluate your shoulder bones on a computer in virtual 3D and planning your shoulder replacement surgery6.
The InSet™ Shoulder System is supported by automated computer-based shoulder arthroplasty planning software called PreView™.
PreView™ software converts your computerized tomography scan (CT scan) into a 3-dimesional computerized replica of your shoulder bones or “glenohumeral joint”.

Then, your shoulder surgeon determines what type and size of implant is best for you.
Your shoulder surgeon also performs a computerized virtual operation to optimize where your implants should be positioned within your glenoid and humeral shoulder bones.

Preserving bone in your first or, primary, reverse shoulder arthroplasty is very important. Sometimes patients need a second reverse shoulder replacement called a revision shoulder arthroplasty (see hyperlink “What are the risks associated with reverse shoulder replacement surgery?”).
Having plenty of bone left to support a new reverse shoulder replacement makes subsequent revision shoulder replacement more straight forward. InSet™ shoulder replacement is bone preserving, saving significant shoulder bone to support future revision shoulder replacement if one is recommended for you.
In addition, bone preserving humeral stems have been shown to reduce shoulder pain after surgery which may result in a quicker shoulder replacement recovery11.
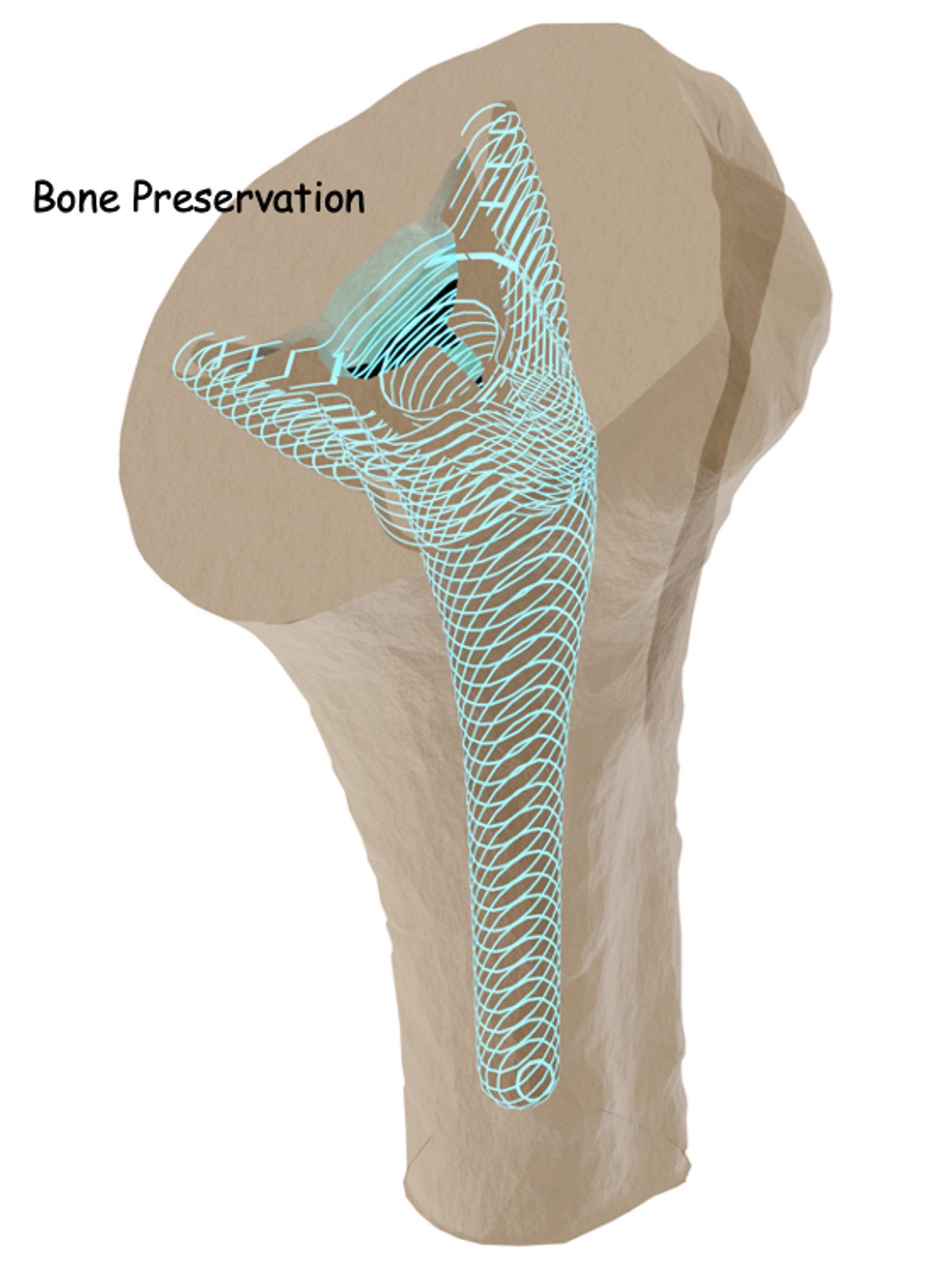
The InSet™ reverse glenoid component includes many different personalized configurations that can significantly reduce the amount of bone removal required for optimal placement within your shoulder joint. These options allow for more straightforward procedures in the future, if they are ever needed.
What to expect before reverse shoulder replacement surgery?
You will meet with your surgeon and review your symptoms and concerns. X-rays will likely be obtained during your visit. You may also be asked to obtain a magnetic resonance imaging scan (MRI scan) and possibly a computerized tomography scan (CT scan). This imaging will give your surgeon an excellent understanding of what’s causing your shoulder pain and any diminished shoulder range of motion. You will also receive a full physical exam.
Once your surgeon determines what is affecting your shoulder, you will likely receive a conservative course of treatment and pain management therapies. Nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids may be prescribed. If your symptoms persist, your surgeon may recommend shoulder replacement surgery.
How to prepare for shoulder replacement surgery?
Your shoulder surgery will be scheduled with advanced notice, and you may be asked to revisit your surgeon once again to review your pre-surgical workup. If you obtained a CT scan, your surgeon may review a 3D surgical plan with you to demonstrate how they determined which implant fits you best!
Several weeks before your shoulder surgery, you may be asked to do basic exercises for your rotator cuff muscles and abstain from any alcohol consumption to help with your shoulder replacement recovery. It is recommended that you talk to your surgeon about any prescribed or unprescribed drugs or narcotics you are taking and follow their instruction carefully. If you smoke, you will be asked to cease smoking because studies have found that smoking can increase your risk for post-operative complications6.
The day before your shoulder replacement surgery, you will likely have to fast, meaning abstaining from eating or drinking most foods and beverages on the eve of your shoulder surgery as prescribed by your doctor. You may also be given a special soap to clean your shoulder.
What to expect on the day of reverse shoulder replacement surgery?
You will be asked to arrive at the hospital or ambulatory surgery center up to two (2) hours prior to your operation. You will complete any remaining paperwork and a nurse will start an IV.
Shoulder replacement is performed under general anesthesia and your anesthesiologist will talk to you about your options and any concerns just prior to your shoulder surgery. You may even be given a local injection to “block” any shoulder pain after your shoulder replacement.
Immediately after your shoulder replacement has been completed, your surgeon will talk to your family and friends, and let them know it’s done, how it went and most importantly, how you are doing.
When you wake up, you will be in a recovery room or recovery area. There, your anesthesia will wear off and you will be stabilized. When you are feeling comfortable, you will be moved to an area or a room where you will be able to see your family and friends.
Before you are discharged from the hospital or ambulatory surgery center (ASC), your shoulder surgeon will talk to you about how your shoulder surgery went, your shoulder replacement recovery, and your overall well-being. You may also work with an occupational or physical therapist who may ask you to perform some movements that will help determine what exercises will be best for you to do during your shoulder replacement recovery.
On the day you are discharged, right before you leave, your shoulder surgeon or a member of his or her staff will check on you and prepare you to leave the facility. Your discharge nurse will go over everything you have to do once you get home.
To make discharge and recovery as comfortable as possible, it’s recommended that you arrange for someone to drive you home and even stay with you for a period of time to help with your daily activities and needs. Arranging for and wearing loose clothing that is easy to take on and off is also a good idea.
What happens after reverse shoulder replacement surgery?
You can expect some shoulder pain. If your shoulder pain is severe enough, you may be offered pain management therapy or prescribed nonsteroidal anti-inflammatory medications (NSAIDs). You will likely also receive antibiotics to reduce the risk of getting an infection at your surgical site. Receiving and using a sling is not uncommon.
Your shoulder replacement recovery starts right away. You will be given a rehabilitation program that includes physical therapy (PT). Your exercises or PT may start very soon after you are discharged but could also start weeks after your operation.
Completing your physical therapy program is essential for regaining strength and motion in your shoulder.
Depending on how your recovery is going, you may expect to return to performing light daily activities two to six weeks after your surgery.
What are the risks associated with reverse shoulder replacement?
Reverse shoulder replacement results are commonly excellent. “Pooled long-term results of reverse total shoulder replacement for massive rotator cuff tears with or without arthritis show significant improvement of overhead function and of objective and subjective outcome scores up to 20 years after surgery”3.
Like all types of surgery, sometimes complications can occur with reverse shoulder replacement. Joint dislocation after reverse shoulder replacement is rare, but considered the most common type of reverse shoulder complication. When it occurs, it is usually treated conservatively, and “reduced” non-surgically, much like any other joint dislocation. If this issue becomes chronic or persistent, surgical intervention will be recommended and the reverse implant may be modified to further stabilize the shoulder.
Other types of complications are similar to most other types of joint replacement like anesthetic complications such as nausea, dizziness and vomiting. Infection of the wound, damage to blood vessels, nerves or muscles, failure to relieve pain, scapula fracture, pulmonary embolism, and wear and tear of prosthesis which may require a repeat surgery are additional potential complications7.
Find A Shoulder Specialist
If you are considering total shoulder replacement surgery, it’s important to see an orthopedic surgeon who specializes in shoulder replacement. Be sure to talk to your shoulder surgeon about all of your questions and concerns. He or she will be able to provide you with more detailed information about shoulder replacement surgery and what you can expect.
- Orthopedic Network News, www.orthopedicnetworknews.com, Volume 31, No. 1, January 2020
- Charles Rockwood, MD, Orthopedics Today, Jan. 01, 2000; https://www.healio.com/news/orthopedics/20120331/a-century-of-shoulder-arthroplasty-innovations-and-discoveries
- Eric T. Ricchetti, Matthew L. Ramsey, CHAPTER 6 – Total Shoulder Arthroplasty, Editor(s): Neil P. Sheth, Jess H. Lonner, Gowned and Gloved Orthopaedics: Introduction to Common Procedures, W.B. Saunders, 2009, Pages 55-69, ISBN 9781416048206
- Gunther SB, Lynch TL, O’Farrell D, Calyore C, Rodenhouse A. Finite element analysis and physiologic testing of a novel, inset glenoid fixation technique. J Shoulder Elbow Surg. 2012 Jun;21(6):795-803. doi: 10.1016/j.jse.2011.08.073. Epub 2011 Dec 14. PMID: 22173268.
- Gunther SB, Tran SK. Long-term follow-up of total shoulder replacement surgery with inset glenoid implants for arthritis with deficient bone. J Shoulder Elbow Surg. 2019 Sep;28(9):1728-1736. doi: 10.1016/j.jse.2019.01.020. Epub 2019 Apr 17. PMID: 31005482.
- https://orthoinfo.aaos.org/en/treatment/surgery-and-smoking/
- Somerson JS, Hsu JE, Neradilek MB, Matsen FA 3rd. Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016. J Shoulder Elbow Surg. 2018 Nov;27(11):1978-1986. doi: 10.1016/j.jse.2018.03.025. Epub 2018 May 11. PMID: 29759905.