We recently had the opportunity to interview Dr. Ryan Churchill, MD and learn more about his background and experiences using InSet™ Systems from Shoulder Innovations in his practice as an orthopedic surgeon. An edited version of our interview led by Dave Blue follows.
Dave Blue:
Dr. Churchill, would you share a little bit about your background including how you became involved in healthcare and specifically in orthopedics?
Dr. Ryan Churchill, MD:
I grew up in New Jersey and went to Villanova for my undergraduate education. I went to Georgetown for medical school and ended up staying at Georgetown in Washington, DC for my residency training. I did my shoulder and elbow fellowship at the Rothman Institute at Thomas Jefferson University Hospital in Philadelphia. When I began my job search I looked from Portland, Maine down to Washington, DC and ended up finding the practice and job that I’m at right now in Peabody, Massachusetts.
With regards to what drew me into medicine, I had a lot of influences and people who were very important to me, who helped to steer that course. In all reality, everything started with my desire to help people. I was able to incorporate that with something I really enjoyed, which was initially science, and eventually medicine.
With regards to orthopedics, it’s a familiar story that you hear from a lot of orthopedists. I had several injuries playing sports (basketball and track in high school), so I was a “frequent flyer” at orthopedic offices. I found that I was drawn to it right from the start, and my passion for it grew over the years. By the time I was a third-year medical student, I knew orthopedics was what I was going to do.
Regarding the shoulder and elbow, I had some influences when I was younger. My dad is a physical therapist, and he specifically does a lot of shoulder therapy. I had a chance to do research with several great shoulder and elbow surgeons in college and I really enjoyed it. I love the shoulder because I think that it is challenging, and it is complicated. I like that it keeps you learning new and better ways of dealing with the problems that arise for patients. Everything isn’t always the same way every time. There are nuances and a complexity to it.
Dave Blue:
Thanks for sharing that. Please share about your journey with using Shoulder Innovations.
Dr. Ryan Churchill, MD:
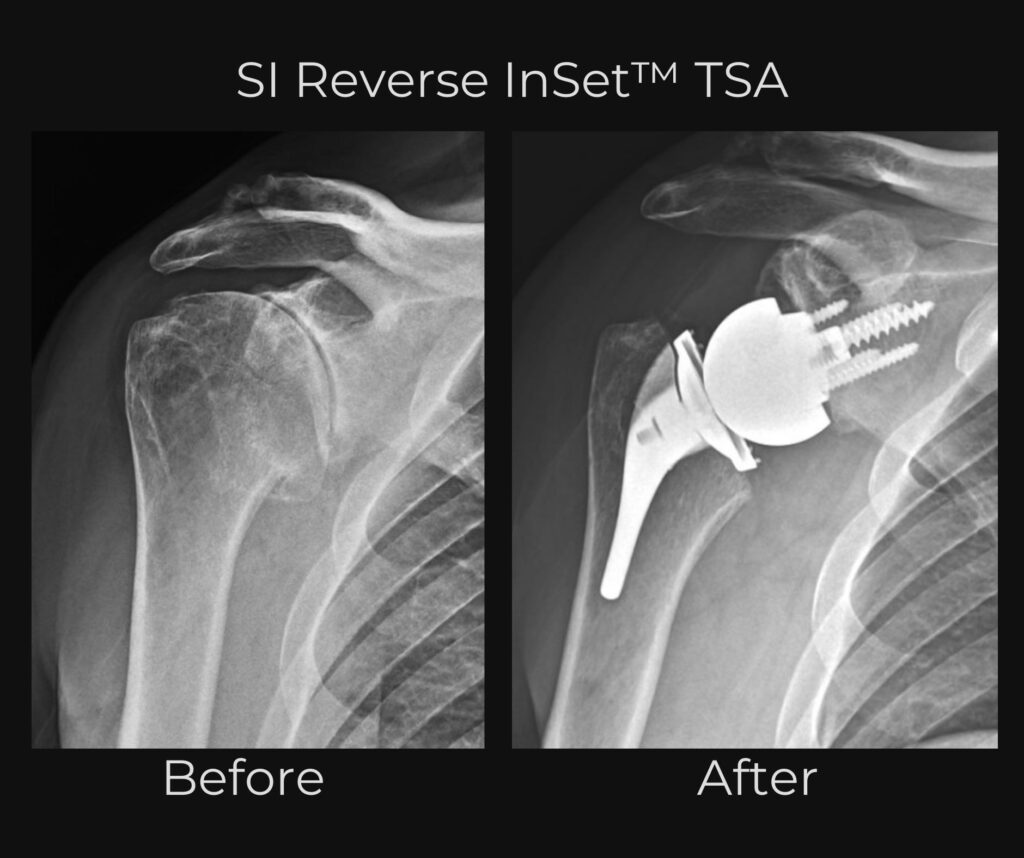
I have been using the InSet™ Total Shoulder Arthroplasty by Shoulder Innovations for at least two and a half years now in my current practice. Recently, this past September, I was able to get the InSet™ Reverse approved for my practice. I was first exposed to Shoulder Innovations in fellowship training. One of my mentors from fellowship used Shoulder Innovations for some of his patients and that was a very big influence on me. We would have discussions about why he used it for the patients he did and it started me thinking more about the benefits of an InSet™ glenoid component.
Dave Blue:
Can you think of any cases in particular or success stories that the patient demonstrated the effectiveness of the InSet™ System? Is there one that stands out?
Dr. Ryan Churchill, MD:
With regards to the Anatomic InSet™ I have numerous patients who I can think of. One patient in particular was a same day surgery. I called him the next day to see how he was doing, and he said, “I feel fine, I’m taking Tylenol and that’s it. This is great!” He cruised along the whole process, and I saw him at his one-year appointment this past December. He has been playing golf the past spring and summer. His forward elevation is to 170 degrees and he has 45-50 degrees of external rotation. He has internal rotation to his lower thoracic spine with great rotator cuff strength, no pain, great motion, and able to do everything that he wants to do without any issue.

With regards to the Reverse, I had a patient recently who was a younger patient (only 59 years old) who had a severe glenohumeral arthritis wear pattern. He had a B3 type glenoid where there is a significant wear of bone on the posterior half of the glenoid. He also had a rotator cuff tear involving his supraspinatus with some extension into his infraspinatus tendon. We talked about all the options and after having a long discussion with him, we ended up going with the Augmented Reverse. I used a 15-degree angle base plate for him, given the degree of deformity he had, and a 39+6 glenosphere. He is only three months out and he can forward elevate to 170 degrees, and externally rotate to 45 degrees. He works in plumbing and he’s itching and ready to get back to his job with literally no pain from the start.
That’s pretty indicative on the whole of how people do after these surgeries. My anatomic patients have really done amazing. And, though it’s only been a little over six months now, I’m seeing the same pattern with my reverse patients.
Dave Blue:
That’s so great to hear! If you were sitting down with a fellow surgeon to walk them through the InSet™ System for the very first time, how would you explain it to them?
Dr. Ryan Churchill, MD:
This system is a very straightforward system and it is easy to use. It’s a single tray for the Anatomic and soon to be a single tray for the Reverse as well. So, everything is contained within one tray and you do not have to go searching through multiple trays to get the instruments that you need. It is very well thought out. And with regards to fixation, you’ll see rock solid fixation for the InSet™ Glenoid for the Anatomic. If you’re using the short stem, or more recently the stemless anatomic, the press fit is amazing! With regards to the Reverse, the instrumentation is very easy and the angled wedge baseplates work very nicely.
Dave Blue:
Do you have any specific tips or tricks that you may share with somebody if they were using the system for the very first time?
Dr. Ryan Churchill, MD:
A tip that I would use for the Anatomic – when you’re getting ready to put your glenoid component in, I would utilize a pen to mark where the pegs are so that you know that you’re orienting the component in the right position. Then once you get it set and in the right spot with the introducer, you can take it off and push it in with your thumb to get it set. Then use the impactor and that’s really all you need. You don’t need to add any more steps to make it more difficult or more complicated.
With regards to the Reverse, one of the pieces of advice I would give involves how to get the glenosphere to sit flush with the baseplate. This is especially useful if you’re utilizing the more lateralized glenosphere. to I will utilize a trial glenosphere to get the angle for glenosphere placement and to ensure I have over tensioned the shoulder. You can then utilize the glenosphere and the inserter handle as a lever to get the glenosphere onto the base plate and get it to seat well.
Dave Blue:
Excellent, do you have any closing thoughts you’d want to add that we haven’t covered already?
Dr. Ryan Churchill, MD:
I think that the future of anatomic shoulder arthroplasty is with the InSet™ System. I think that we are going to see a continued increase in the use of the reverse as patient outcomes continue to improve. Overall I feel that the trend in shoulder arthroplasty is going to depend on glenoid deformity, status of the rotator cuff and patient age. Patients with A1, A2, B1, B2, and C wear patterns with an intact rotator cuff and of appropriate age are going to be Anatomics. In those situations, I think that the options you have with the InSet™ can make up for any deformity you have. In the situation of a type C, you can play it where it lies because that is where that patient’s soft tissue tension has developed. In general (and this is my own personal opinion) I believe that theB3 glenoids with significant deformity are going to be Reverses as that will be the more reproducible outcome for the patient.
That being said I think that for shoulder arthroplasty patients the InSet™ is the future because when you put the glenoid in, the fixation is extremely solid from time zero. Personally, I let my active patients go back to doing push-ups, pull ups, and bodyweight exercises, because of how confident I feel in the fixation. I believethat this is the next step in shoulder arthroplasty, specifically for the anatomic patients.This system not only has the tools to correct deformity and restore motion, but it takes it one step further with the activity level patients can return to with the confidence you have in the glenoid fixation. With the design of this implant you are not going to get the rocking horse phenomenon. You are not going to get glenoid loosening. We can really let patients be as active as they wish to be.
Dave Blue:
Thank you again so much for taking this time Dr. Churchill, I really appreciate it.
Dr. Churchill is an orthopedic surgeon in Peabody, MA

