Total Shoulder Replacement
What to know about anatomic shoulder replacement surgery
A Patient’s Guide
Benefits to total shoulder replacement surgery may include:
- May relieve your shoulder pain and improve your shoulder motion.
- May return you to your normal daily activities and active lifestyle.
Over the past 15 years, total shoulder replacement, also known as total shoulder arthroplasty, has advanced significantly. Surgeons cannot only relieve your shoulder pain, but they can also:
- More accurately restore your normal shoulder anatomy to help you achieve excellent shoulder movement or “range of motion.”
- Preserve more of your shoulder bone should future shoulder replacement surgery be necessary.
- Get you back to your normal daily activities and active lifestyle.
This guide answers common questions about shoulder replacement surgery:
- What makes up your shoulder anatomy?
- What conditions may be treated with shoulder replacement?
- How may you benefit from shoulder replacement surgery?
- What is the difference between a total shoulder and a reverse shoulder replacement surgery?
- How the latest advancements in shoulder replacement may benefit you?
- What to expect if you decide to have shoulder replacement surgery?
- How to find a surgeon that specializes in shoulder surgery utilizing the advancements in this guide.
What makes up your shoulder anatomy?
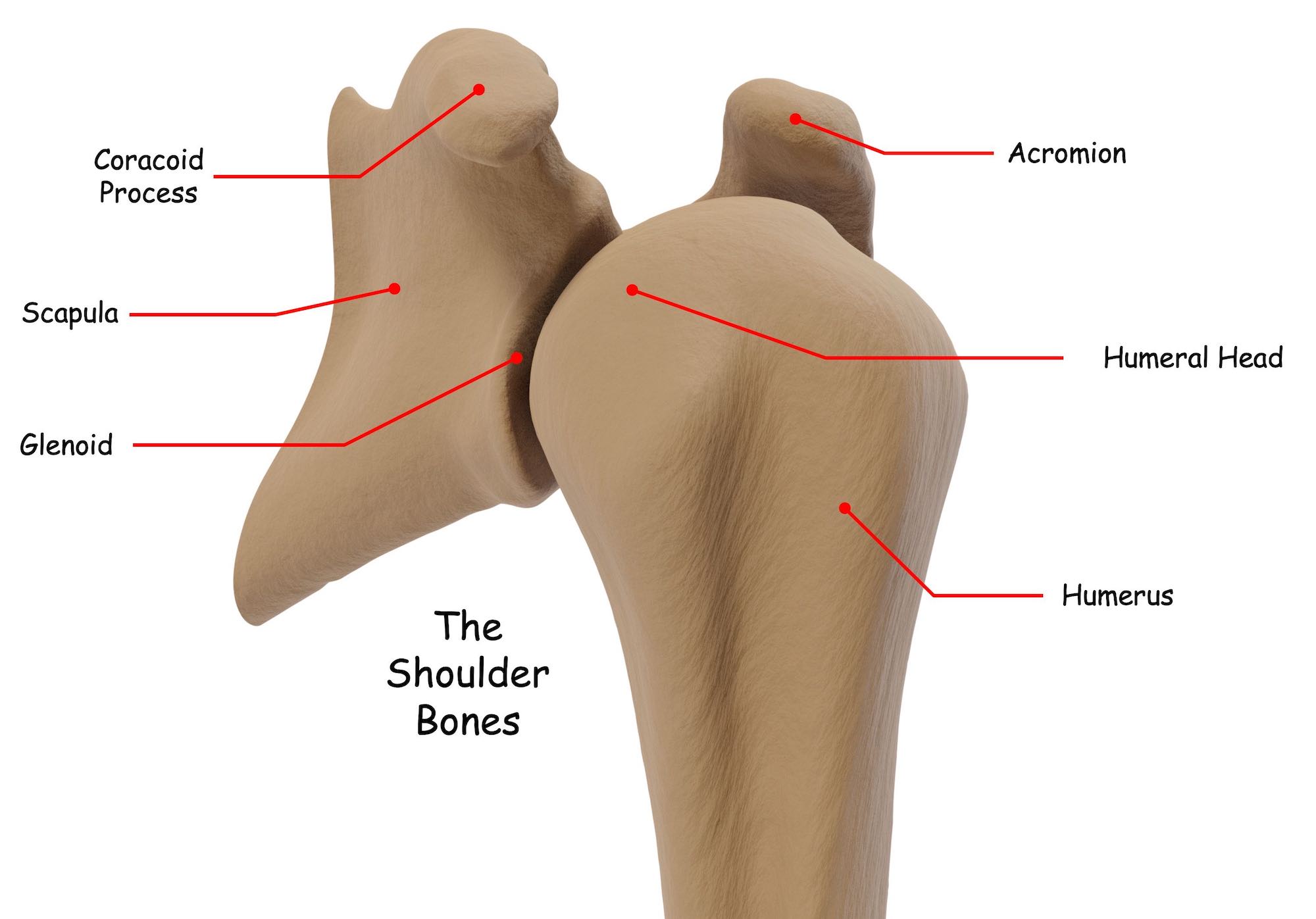
- The humerus, scapula, and clavicle make up your shoulder joint.
- The shoulder is a ball and socket joint that allows motion in all directions.
- The rotator cuff stabilizes and moves your shoulder bones.
Your shoulder joint or “glenohumeral joint” is one of the more complex joints in your body.
Three shoulder bones make up the shoulder joint; the humerus, also known as the long bone of the upper arm, the scapula or shoulder blade, and the clavicle, sometimes referred to as the collar bone.
Your shoulder is a ball and socket joint. Ball and socket joints allow movement in all directions. In your shoulder joint, the upper part of the humerus or humeral head is the “ball,” and a part of your scapula called the glenoid is the “socket.”
Both the humeral head and the glenoid have a smooth lining called articular cartilage. The articular cartilage allows the shoulder to move smoothly, efficiently, and painlessly.
The shoulder joint is stabilized by a group of tendons, called the rotator cuff, that encapsulates the shoulder joint as well as a large muscle called the deltoid. In addition to stabilizing the shoulder bones, shoulder motion or mobility is generated by these tendons and muscles. In fact, the shoulder joint is one of the most mobile joints in the human body!
What common shoulder joint conditions are treated with total shoulder replacement surgery?
- Shoulder pain caused by shoulder arthritis.
- Rheumatoid arthritis in the shoulder joint.
Over time the smooth lining or articular cartilage of the humeral head and glenoid wears. They can even wear out completely. As years go by, the articular cartilage thins and breaks down to a point where smooth, efficient, pain-free movement is no longer possible. Generally, when the articular surface wears out, you may experience shoulder pain and possibly restricted shoulder movement. This condition is called shoulder arthritis, and it is one of the most common reasons a surgeon would recommend a total shoulder replacement surgery. It is caused by wear and tear on the shoulder joint over many years of use.
Sometimes, total shoulder replacement surgery is referred to as “total shoulder arthroplasty” or “anatomic shoulder replacement.”
There are other forms of arthritis. A less common form is rheumatoid arthritis. This is a condition where chemicals are created by the body’s immune system that attacks the cartilage. It can affect any joint in the human body and more commonly affects women.
Another way arthritis can occur is if there was a previous injury to the shoulder. Injuries like a torn rotator cuff or torn ligaments, as well as shoulder fractures, can, over time, cause inconsistencies in the smooth articular surfaces of the shoulder, making the shoulder bones more susceptible to arthritis. This condition is called post-traumatic arthritis.
How is shoulder arthritis treated?
- Initially, with non-surgical treatments like physical therapy and reduced activity.
- For more acute shoulder pain, nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids may be prescribed.
- For severe shoulder pain, shoulder replacement surgery may be recommended.
Shoulder arthritis is painful, and your shoulder pain can become more severe over time, limiting what you can do with your shoulder. Typically, non-surgical treatments are recommended first.
Certain types of physical activities may be limited or restricted, and physical therapy may be prescribed. Physical therapy is essential when treating shoulder arthritis and can be an effective way to reduce pain, improve shoulder motion and delay surgical intervention. As your shoulder pain becomes more severe, nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids may be prescribed. Corticosteroids are powerful anti-inflammatory drugs that can be taken by mouth or injected into your shoulder.
When conservative, non-surgical treatments no longer provide adequate pain relief and daily activities like getting a good night’s sleep, getting dressed, brushing your teeth, combing your hair, reaching behind your back as well as playing golf, tennis, and other similar activities become difficult or impossible, a shoulder replacement surgery may be recommended. When both shoulder joint surfaces are replaced, it is called total shoulder replacement or total shoulder arthroplasty. When only one surface or “half” of your shoulder joint (the humerus or humeral bone) is replaced, it is called hemi shoulder replacement or hemi shoulder arthroplasty.
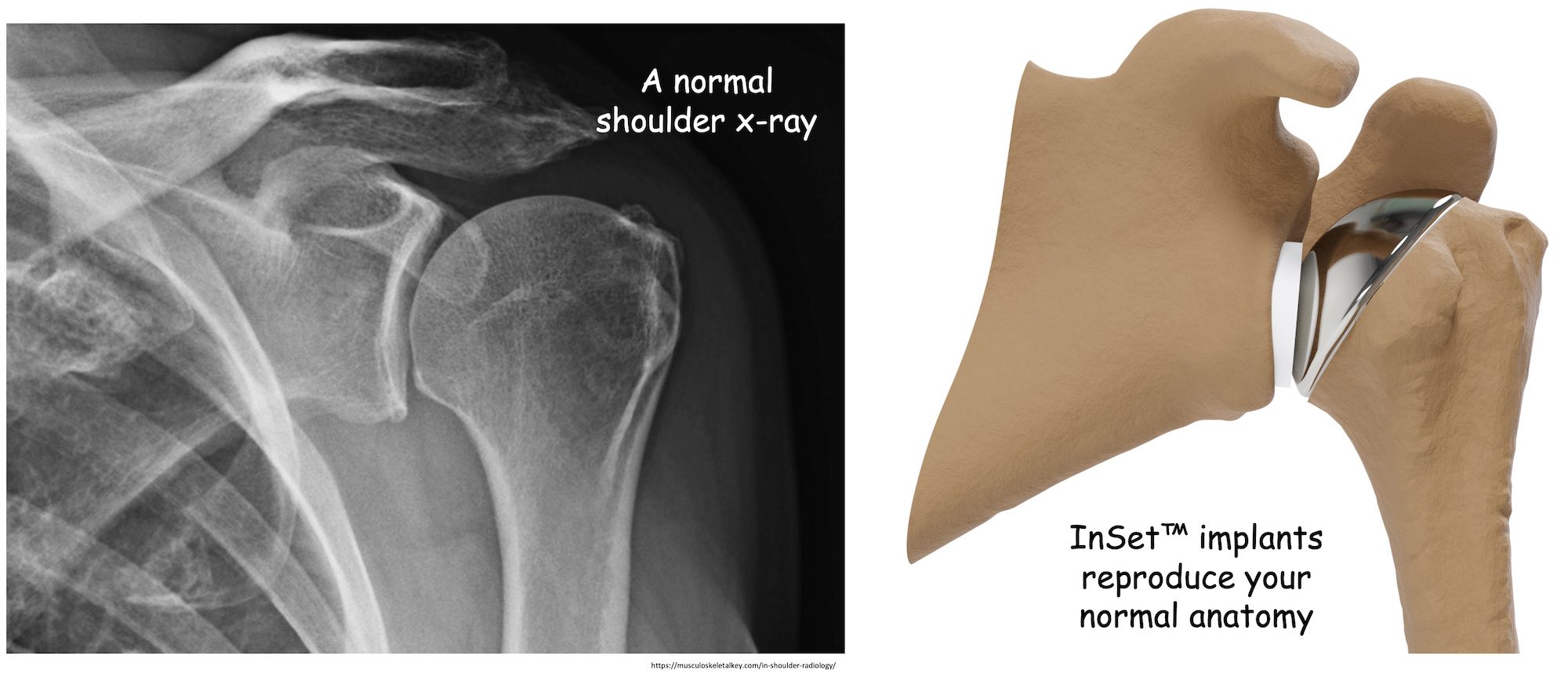
You may even hear your surgeon refer to your total shoulder arthroplasty or hemi shoulder arthroplasty as an “anatomic shoulder .”Anatomic shoulder implants are commonly utilized to treat different types of shoulder arthritis. The idea is to restore your shoulder bones to their normal or “anatomic” shapes.
On occasion, if you are elderly, your surgeon may recommend “reverse shoulder replacement” for severe shoulder pain caused by arthritis. Please see the reverse shoulder replacement surgery section.
After shoulder replacement surgery and a full recovery, your shoulder joint should glide smoothly, efficiently, and, in some cases, without pain once again. Then, you can return to most or sometimes all your normal daily activities.
How may you benefit from total shoulder replacement surgery for arthritis?
- Reduced shoulder pain.
- Improved strength and shoulder motion.
- A return to normal daily activities and a more active lifestyle.
After complete recovery from shoulder replacement surgery, you should experience reduced shoulder pain, improved strength, and improved shoulder motion or range of motion (ROM)1.
Most importantly, after shoulder arthroplasty, you may eventually return to normal daily activities like sleeping comfortably, getting dressed, playing golf and tennis, as well as other physical necessities and activities!1

What advanced total shoulder replacement technology can benefit you today?
InSet™ Total Shoulder Replacement
- Replicates your normal shoulder joint to help you achieve your best shoulder motion.
- Offers shoulder replacement options to treat your individual shoulder anatomy and condition.
- May improve how long your total shoulder arthroplasty lasts.
- Engineered with your future in mind.
InSet™ total shoulder replacement replicates your normal shoulder anatomy
- Restores your shoulder anatomy and rotator cuff balance.
- Helps you achieve your best range of motion.
- May reduce your risk for future complications.
The InSet™ Shoulder Replacement System is made of titanium alloy and is engineered to accurately restore the natural shape of your shoulder bones and balance of your shoulder joint and rotator cuff, which is essential for achieving your best possible motion and durability.
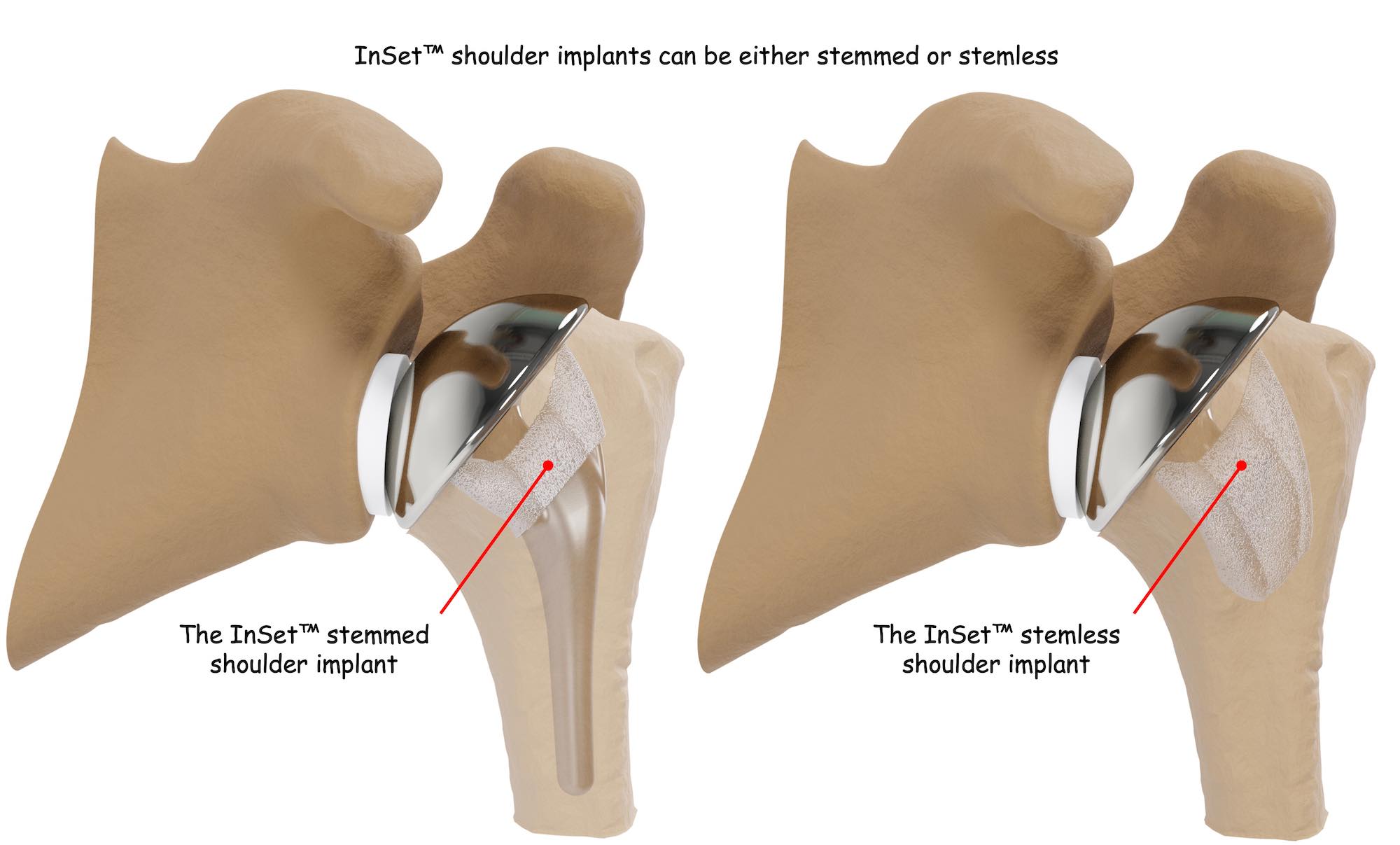
InSet™ total shoulder replacement implant options match your unique condition and bone quality
- InSet™ short stem shoulder replacement
- InSet™ stemless shoulder replacement
There are two InSet™ total shoulder replacement implant options for anatomic shoulder arthroplasty: short stem shoulder replacement and stemless shoulder replacement. Your surgeon will determine which configuration is best for you based on your individual anatomy and condition.
InSet™ total shoulder replacement implants are designed to be durable
- Designed to address the most common reason for a revision shoulder surgery
- Engineered, tested, and studied to help improve durability over time
- Glenoid implants are uniquely placed within the strongest bone of your shoulder.
- Humeral implants are made of titanium alloy and shaped to fit securely within your shoulder bone.
- Optimized in 3D by your surgeon to fit your personal shoulder anatomy with automated computerized software.
Total shoulder replacement surgery is a very effective operation for restoring shoulder movement and reducing or eliminating shoulder pain. But these outcomes are not guaranteed to last long term. Approximately 90% or more of patients can be expected to attain good or excellent pain relief following anatomic total shoulder replacement, and implant survivorship (how long the implant lasts) is greater than 90% at ten years8. This means that total shoulder arthroplasty is usually very effective, but sometimes people need a second shoulder replacement.
How long total shoulder replacement implants last can, in part, depend on how stable each of the components remains over time.
The most common reason for requiring a second shoulder replacement surgery is glenoid implant loosening, in other words, an unstable glenoid component. When this happens, you may experience shoulder pain, loss of movement, or even a clunking or noise sensation8. If you are under the age of 55, the survival rate of the glenoid component can drop to just 62% after ten years9.
The InSet™ glenoid implant is engineered to reduce the potential for loosening. Its unique design and how it is placed within your shoulder bone makes it significantly more stable than common or “traditional” glenoid implants.

Unlike traditional glenoid implants that are placed on top of your glenoid surface, the InSet™ glenoid implant is placed within the most supportive bone of your glenoid. When this is done, stress that contributes to loosening is significantly reduced4.
Fact: Testing shows stress on the InSet™ glenoid implant is reduced by 87% when compared to traditional glenoid implants.4
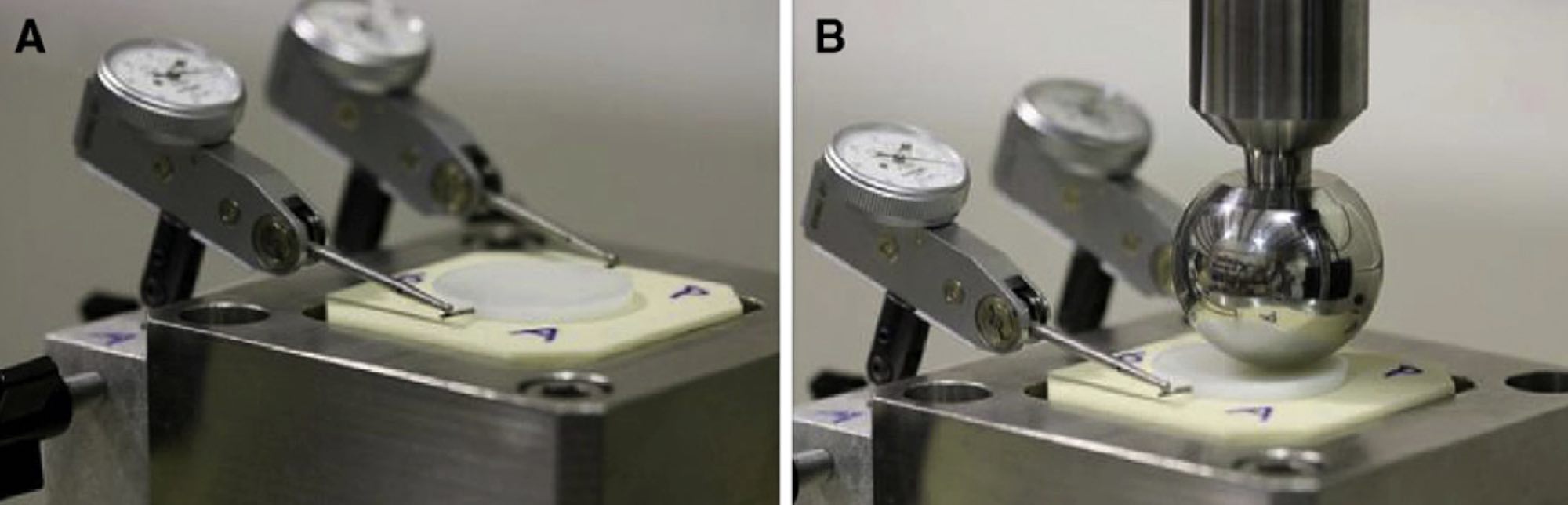
Reducing stress on the glenoid implant can increase how long the component lasts, and the InSet™ is backed by promising data that supports its long-term durability.5
Fact: Two long-term studies show an improved range of motion, no loosening or complications when the Inset™ glenoid component is used for anatomic shoulder replacement!5,10
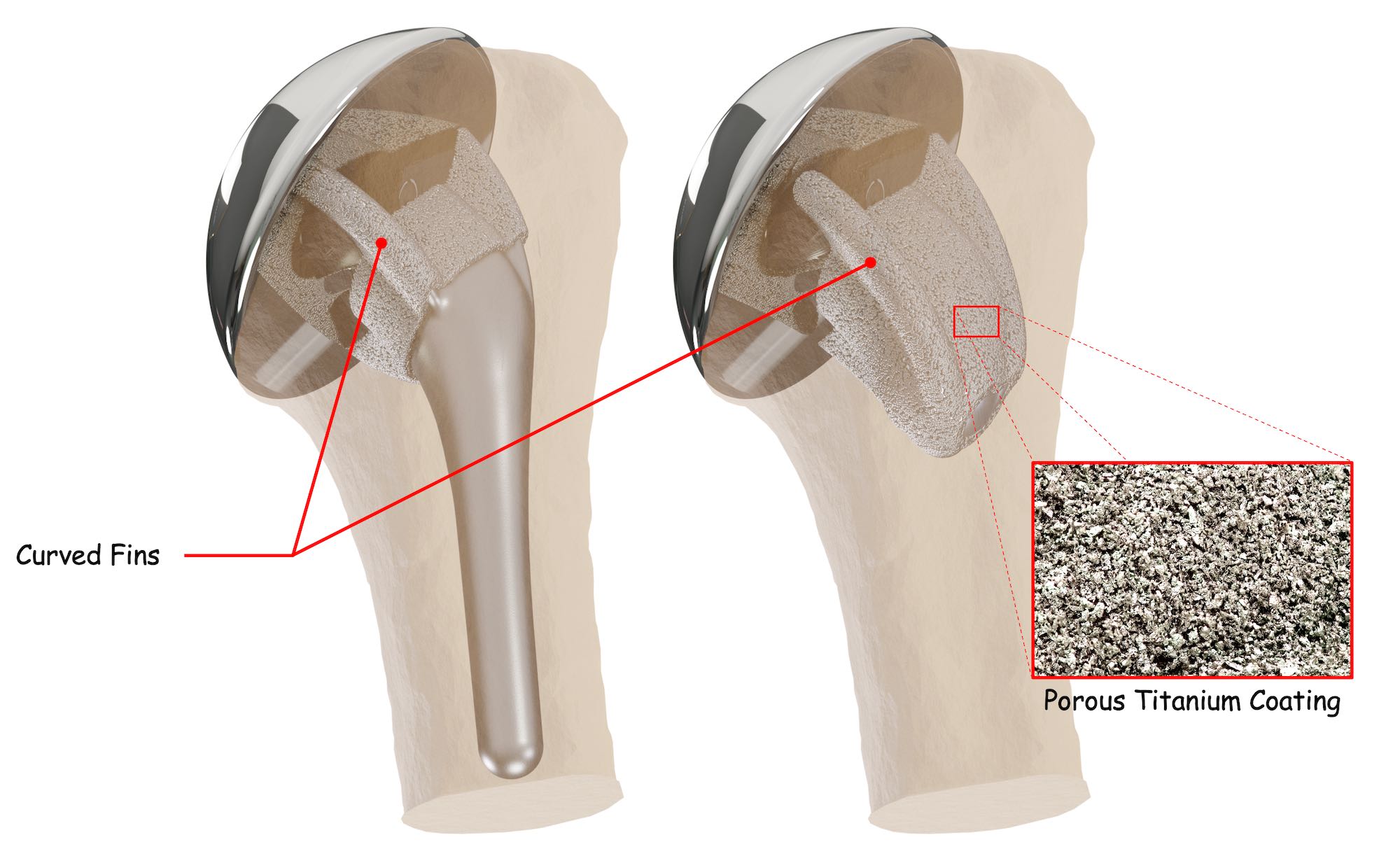
The InSet™ titanium humeral stems feature three unique fins curved and coated with a rough titanium bone-friendly material that promotes mechanical fixation through bone growth into the pores of a rough surface coating, referred to as “bony ingrowth.” This can improve stem security within your shoulder bone3. Together, these two features work to help improve the humeral implant’s stability as well as its durability.
Another way to improve the longevity of a shoulder replacement is for your surgeon to evaluate your shoulder bones on a computer in virtual 3D and plan your shoulder replacement surgery6.
The InSet™ Shoulder System is supported by automated computerized shoulder arthroplasty planning software called PreView™.
PreView™ software converts your computerized tomography scan (CT scan) into a 3-dimensional computerized replica of your shoulder bones.

Then, your shoulder surgeon determines what type and size implant is best for you.
Your shoulder surgeon also performs a virtual shoulder surgery to optimize where your implants should be positioned within your glenoid shoulder bone.

InSet™ total shoulder replacement implants are designed with your future in mind
InSet™ shoulder replacement simplifies the number of steps needed to perform shoulder replacement surgery.
- Your time in surgery may be reduced
- Your blood loss and risk for complications while in surgery may be reduced11
InSet™ total shoulder implants preserve your shoulder bone.
- Improved support for a second shoulder replacement.
- Your shoulder replacement recovery may be faster due to less shoulder pain11
If a second shoulder replacement is needed, your surgeon may be able to preserve your existing humeral implant.
Preserving bone in your first or primary shoulder arthroplasty is very important. Sometimes patients need a second shoulder replacement called a revision shoulder arthroplasty.
Having plenty of bone left to support a new shoulder implant makes subsequent revision shoulder replacement more straightforward. InSet™ shoulder replacement is bone preserving, saving significant shoulder bone to support a revision shoulder replacement if one is recommended for you.
In addition, bone-preserving humeral stems have been shown to reduce shoulder pain after shoulder surgery which may result in a quicker shoulder replacement recovery11.
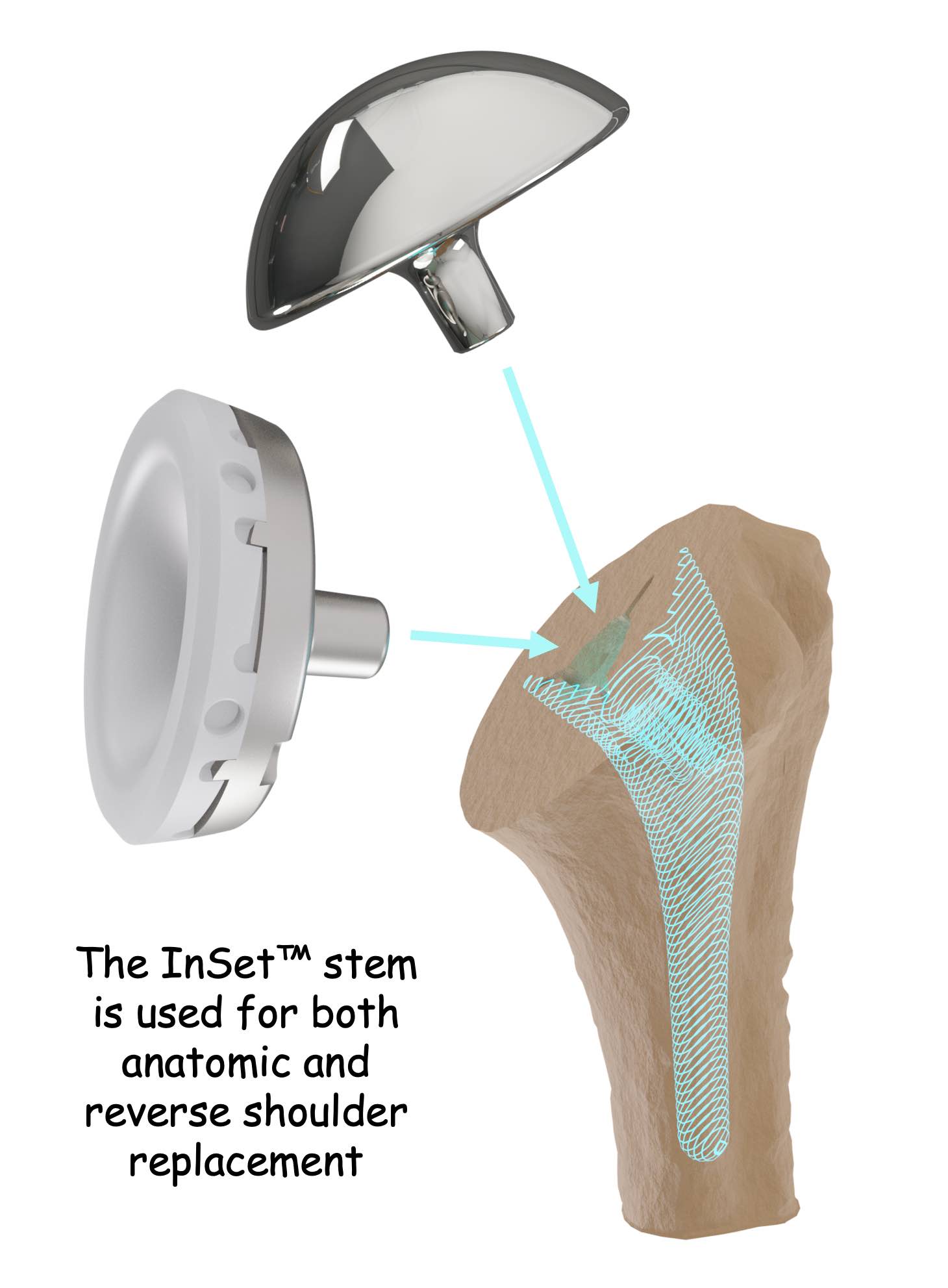
If you ever need a second shoulder replacement, your InSet™ total shoulder arthroplasty or hemi shoulder arthroplasty can be changed or “converted” to a reverse shoulder replacement, the most common type of shoulder implant recommended after anatomic shoulder replacement.
Retaining the original InSet™ humeral stem usually makes the second shoulder replacement more straightforward when compared to shoulder implants that require complete humeral stem removal.
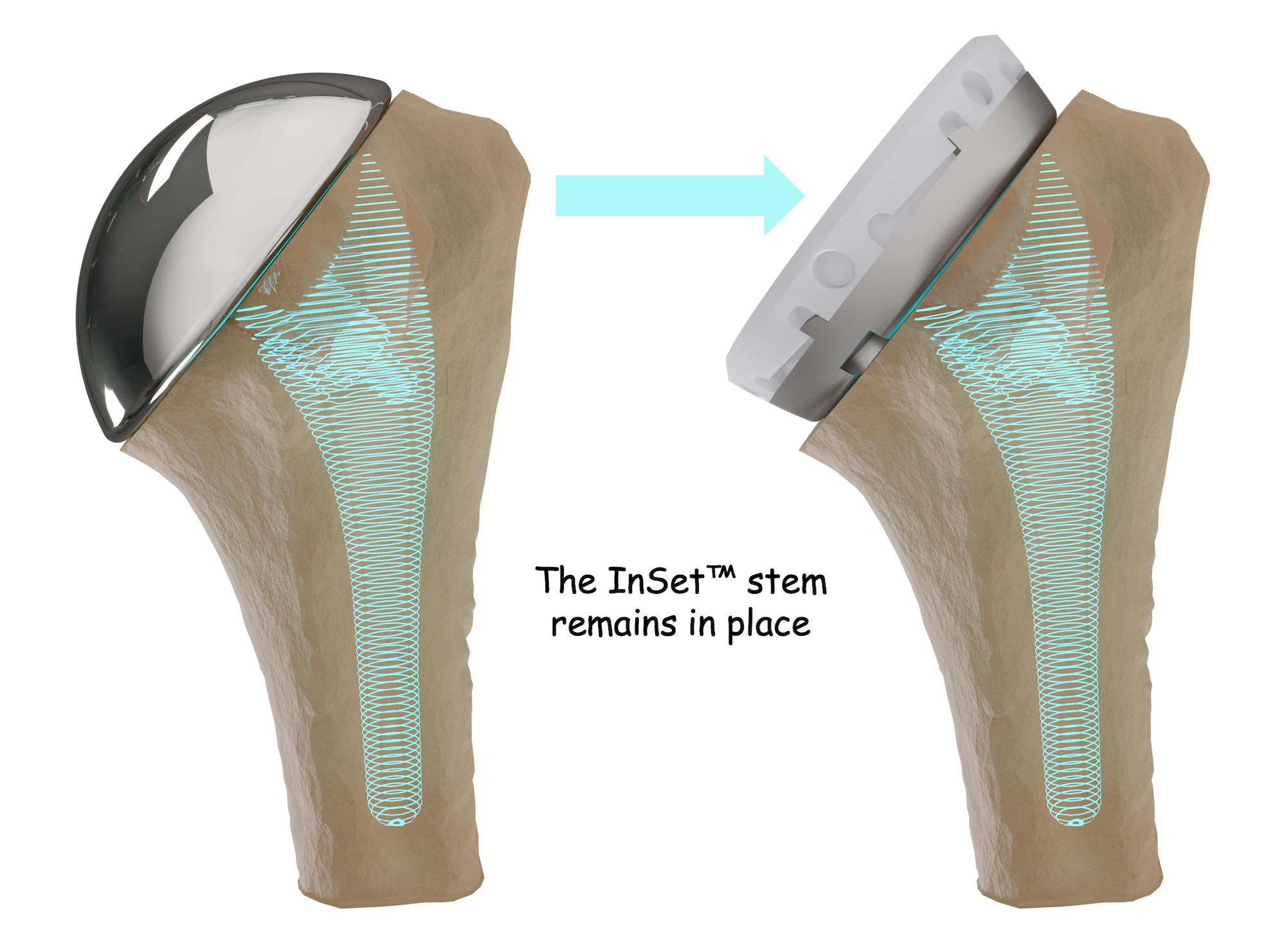
The specialized design of the InSet glenoid implant simplifies the steps required to exchange your original implant for an InSet™ reverse glenoid implant.
Reducing the number of steps required to exchange your original total shoulder replacement implants may reduce the amount of time needed for your second shoulder replacement surgery.
Reducing the amount of time you spend in surgery may reduce your amount of blood loss during surgery as well as shoulder pain after surgery. 11
What to expect before shoulder replacement surgery?
You will meet with your surgeon and review your symptoms and concerns. X-rays will likely be obtained during your visit. You may also be asked to obtain a magnetic resonance imaging scan (MRI scan) and possibly a computerized tomography scan (CT scan). This imaging will give your surgeon an excellent understanding of what’s causing your shoulder pain and any diminished shoulder range of motion. You will also receive a full physical exam.
Once your surgeon determines what is affecting your shoulder, you will likely receive a conservative course of treatment and pain management therapies. Nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids may be prescribed. If your symptoms persist, your surgeon may recommend shoulder replacement surgery.
How to prepare for shoulder replacement surgery?
Your shoulder surgery will be scheduled with advanced notice, and you may be asked to revisit your surgeon once again to review your pre-surgical workup. If you obtained a CT scan, your surgeon may review a 3D surgical plan with you to demonstrate how they determined which implant fits you best!
Several weeks before your shoulder surgery, you may be asked to do basic exercises for your rotator cuff muscles and abstain from any alcohol consumption to help with your shoulder replacement recovery. It is recommended that you talk to your surgeon about any prescribed or unprescribed drugs or narcotics you are taking and follow their instruction carefully. If you smoke, you will be asked to cease smoking because studies have found that smoking can increase your risk for post-operative complications.
The day before your shoulder replacement surgery, you will likely have to fast, meaning abstaining from eating or drinking most foods and beverages on the eve of your shoulder surgery as prescribed by your doctor. You may also be given a special soap to clean your shoulder.
What to expect on the day of shoulder replacement surgery?
You will be asked to arrive at the hospital or ambulatory surgery center up to two (2) hours prior to your operation. You will complete any remaining paperwork, and a nurse will start an IV.
Shoulder replacement is performed under general anesthesia, and your anesthesiologist will talk to you about your options and any concerns just prior to your shoulder surgery. You may even be given a local injection to “block” any shoulder pain after your shoulder replacement.
Immediately after your shoulder replacement has been completed, your surgeon will talk to your family and friends, and let them know it’s done, how it went, and most importantly, how you are doing.
When you wake up, you will be in a recovery room or recovery area. There, your anesthesia will wear off, and you will be stabilized. When you feel comfortable, you will be moved to an area or a room where you can see your family and friends.
Before you are discharged from the hospital or ambulatory surgery center (ASC), your shoulder surgeon will talk to you about how your shoulder surgery went, your shoulder replacement recovery, and your overall well-being. You may also work with an occupational or physical therapist who may ask you to perform some movements that will help determine what exercises will be best for you to do during your shoulder replacement recovery.
On the day you are discharged, right before you leave, your shoulder surgeon or a member of their staff will check on you and prepare you to leave the facility. Your discharge nurse will review everything you must do once you get home.
To make discharge and recovery as comfortable as possible, it’s recommended that you arrange for someone to drive you home and even stay with you for a period of time to help with your daily activities and needs. Arranging for and wearing loose clothing that is easy to take on and off is also a good idea.
What happens after shoulder replacement surgery?
You can expect some shoulder pain. If your shoulder pain is severe enough, you may be offered pain management therapy or prescribed nonsteroidal anti-inflammatory medications (NSAIDs). You will likely also receive antibiotics to reduce the risk of getting an infection at your surgical site. Receiving and using a sling is not uncommon.
Your shoulder replacement recovery starts right away. You will be given a rehabilitation program that includes physical therapy (PT). Your exercises or PT will start very soon after you are discharged.
Completing your physical therapy program is essential for regaining strength and motion in your shoulder.
Depending on how your recovery is going, you may expect to return to performing light daily activities two to six weeks after your surgery.
What are the risks associated with total shoulder replacement surgery?
Total shoulder replacement is a very effective operation for restoring shoulder movement and reducing or eliminating shoulder pain.
Clinical data shows that approximately 90% or more of patients can be expected to attain good or excellent pain relief following total shoulder arthroplasty, and implant survivorship (how long your shoulder replacement lasts) is greater than 90% at ten years7.
Occasionally there can be complications. Anesthetic complications such as nausea, dizziness, and vomiting may occur. Though unlikely, allergic reactions or sensitivities to materials, bone fracture, loss of implant fixation, reduced range of motion, arm length shortening, or device fracture are all potential complications associated with a shoulder replacement. Infection of the wound and dislocation also may happen. Other complications might include damage to blood vessels, nerves, or muscles, failure to relieve shoulder pain, pulmonary embolism, and wear and tear on the implants, which may require a repeat or “revision” surgery. These types of complications are not common.
Find A Shoulder Specialist
If you are considering total shoulder replacement surgery, it’s important to see an orthopedic surgeon who specializes in shoulder replacement. Be sure to talk to your shoulder surgeon about all of your questions and concerns. They will be able to provide you with more detailed information about shoulder replacement surgery and what you can expect.
References
- Orthopedic Network News, www.orthopedicnetworknews.com, Volume 31, No. 1, January 2020
- Charles Rockwood, MD, Orthopedics Today, Jan. 01, 2000; https://www.healio.com/news/orthopedics/20120331/a-century-of-shoulder-arthroplasty-innovations-and-discoveries
- Carpenter SR, Urits I, Murthi AM. Porous metals and alternate bearing surfaces in shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016 Mar;9(1):59-66. doi: 10.1007/s12178-016-9319-x. PMID: 26797775; PMCID: PMC4762800.
- Gunther SB, Lynch TL, O’Farrell D, Calyore C, Rodenhouse A. Finite element analysis and physiologic testing of a novel, inset glenoid fixation technique. J Shoulder Elbow Surg. 2012 Jun;21(6):795-803. doi: 10.1016/j.jse.2011.08.073. Epub 2011 Dec 14. PMID: 22173268.
- Gunther SB, Tran SK. Long-term follow-up of total shoulder replacement surgery with inset glenoid implants for arthritis with deficient bone. J Shoulder Elbow Surg. 2019 Sep;28(9):1728-1736. doi: 10.1016/j.jse.2019.01.020. Epub 2019 Apr 17. PMID: 31005482.
- What is the deviation in 3D preoperative planning software? A systematic review of concordance between plan and actual implant in reverse total shoulder arthroplasty, Lilley, Brendan M. et al., Journal of Shoulder and Elbow Surgery, Volume 31, Issue 5, 1073 – 1082
- Eric T. Ricchetti, Matthew L. Ramsey, CHAPTER 6 – Total Shoulder Arthroplasty, Editor(s): Neil P. Sheth, Jess H. Lonner, Gowned and Gloved Orthopaedics: Introduction to Common Procedures, W.B. Saunders, 2009, Pages 55-69, ISBN 97814160482068Frederick A. Matsen, III, Jeremiah Clinton, Joseph Lynch, Alexander Bertelsen and Michael L. Richardson J Bone Joint Surg Am. 2008;90:885-896. doi:10.2106/J BJS.G.01263
- Mid- to long-term follow-up of total shoulder arthroplasty using a keeled glenoid in young adults with primary glenohumeral arthritis Denard, Patrick J. et al. Journal of Shoulder and Elbow Surgery, Volume 22, Issue 7, 894 – 900
- Total shoulder arthroplasty using an inlay glenoid component for glenoid deficiency: mid- to long-term follow-up of a previously published cohort Rondon, Alexander J. et al. Journal of Shoulder and Elbow Surgery, Volume 0, Issue 0
- Churchill R., Clinical and radiographic outcomes of the simpliciti canal-sparing shoulder arthroplasty system: a prospective two-year multicenter study. J Bone Joint Surg Am. 2016;98:552-60
